Abstract
Background: Heparin induced thrombocytopenia (HIT) is a life-threatening complication of heparin exposure. It is characterized by the production of heparin-platelet factor 4 (PF4) antibodies, leading to drug-dependent platelet activation, thrombocytopenia and thrombosis. Current guidelines recommend pursuing laboratory diagnosis of HIT based on validated clinical scoring criteria such as the 4T score. Those with a 4T score ≥4 are considered to have moderate probability of HIT and should undergo laboratory screening via ELISA for detection of anti-PF4/heparin antibodies, which is measured quantitatively in terms of optical density (OD). This test is readily available, highly sensitive (100% in multiple prospective studies) and results are typically available within 24 hours, making it an optimal screening test; however, its specificity is limited (81-89%) (Bakchoul 2009; Pouplard 2007). The serotonin release assay (SRA) is a functional assay with a high specificity and sensitivity for HIT and is therefore considered the gold standard of diagnosis; however, its use is limited by cost, availability, and prolonged time for results. Guidelines recommend treatment with a non-heparin anticoagulant immediately in those with a 4T score of ≥4 while other tests are pending. A common cutoff for ELISA OD positivity has been 0.4, which is based on control groups from healthy donors and may not reflect hospitalized patients. Several studies have shown that increasing the OD threshold may preserve sensitivity while increasing the positive predictive value (PPV), thereby reducing morbidity associated with overdiagnosis (Warkentin 2008; Chan 2015). In the current study, we evaluated the effect of combining 4T score with ELISA OD to improve diagnostic precision for the diagnosis of HIT.
Methods: This is a retrospective chart review of patients who had a positive HIT polyspecific ELISA (correlating to an OD ≥0.4) from 1/1/2016 to 7/2/2020 at a large urban academic center. 4T scores were calculated retrospectively by trained investigators using chart information available to clinicians at the time the ELISA was sent. For the purposes of data analysis, patients who did not have an SRA sent, had an indeterminant SRA or had an incomplete inpatient chart were excluded. SRA positivity was considered confirmatory of a HIT diagnosis.
Results: 260 patients had a HIT ELISA OD ≥0.4. 183 patients were included in the final analysis. Median age was 63 (21-92) and the male/female ratio was 1.29. 123 (67%) were in an ICU when HIT was suspected. 10 patients were COVID positive ≤14 days prior to the HIT ELISA. 84 patients (46%) were receiving thromboprophylaxis dosed heparin products, while 99 (67%) were on full dose anticoagulation. 162 (89%) were receiving heparin at the time of testing, while 21 (11%) were receiving enoxaparin. Median 4T score was 4 (range 1-8) and median OD was 0.76 (range 0.41-3.52). SRA was positive in 43 patients (23%).
The predictive value of the 4T score for SRA positivity was calculated for 4T score cutoffs of 4, 5 and 6. PPV was 0.29 (95% CI 0.22-0.38), 0.37 (95% CI 0.27-0.48) and 0.55 (95% CI 0.36-0.74), and negative predictive value (NPV) was 1.00 (95% CI 0.91-1.00), 0.90 (95% CI 0.82-0.95) and 0.82 (95% CI 0.76-0.88), respectively. 0 of 37 patients with a 4T score less than 4 had a positive SRA.
The predictive value of the HIT ELISA was also examined. Increasing the OD cutoff from >0.4 to >0.7 maintained 100% sensitivity for HIT (95% CI 0.92, 1.00), with a NPV of 1.0 (95% CI 0.96, 1.00), while increasing the PPV from 0.24 to 0.45 (95% CI 0.35, 0.56). OD of >2.8 was 100% specific for HIT (95% CI 0.97-1.00) with a PPV of 1.0 (95% CI 0.69-1.00) (n=10).
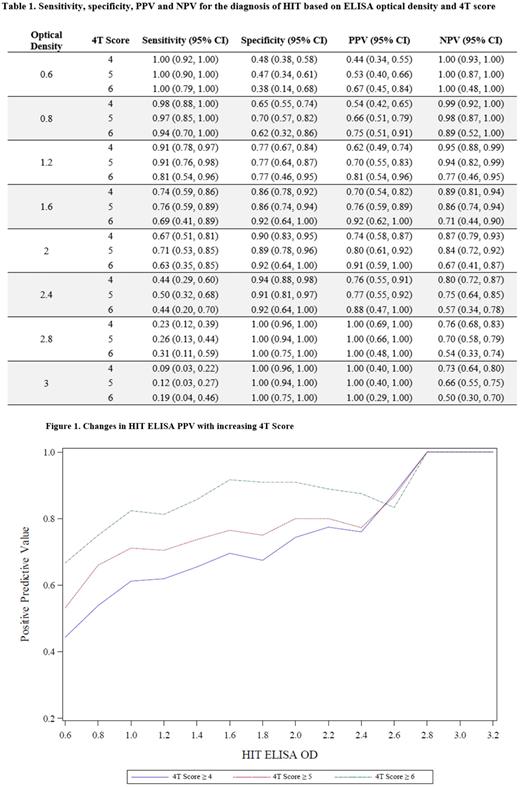
We then determined the relative sensitivity, specificity, PPV and NPV for ELISA among 3 groups of patients with a 4T score of ≥4 (n=146), ≥5 (n=91) and ≥6 (n=29) (Table 1). Higher 4T cutoffs increased the relative PPV for OD until approximately OD of 2.6, at which point 4T cuts at 4, 5, or 6 no longer increased PPV (Figure 1). Conversely, NPV declined with increasing 4T cutoffs.
Conclusion: Our data suggests that increasing the HIT polyspecific ELISA OD cutoff for positivity from 0.4 to 0.7 maintains a sensitivity of 100% for the diagnosis of HIT, while increasing the PPV. Combining 4T score with OD increases the PPV for OD ranges up to approximately OD of 2.6 after which 4T score did not add predictive value. Our study was limited by number of patients (particularly with 4T scores of 6 or greater).
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.